The Gut-Brain Connection & Mental Health
What do you think of when you hear the words “bacteria, viruses, and fungi”? These terms often conjure ideas of filth and disease, but you might be shocked to learn that almost every centimeter of our bodily surfaces hosts entire ecosystems of bacteria, viruses, and fungi. We are home to trillions of these microbes, with them outnumbering our own cells by 10 to 1. In fact, these microorganisms are essential to our overall health!
These microbes and their genetic materials are collectively called a microbiome. Our largest and most diverse microbiome is located within our gut, and these bugs aid in the normal digestion of foods. You may have seen products called probiotics popping up on grocery store shelfs? Probiotics contain live and active bacteria believed to aid in healthy gut function.
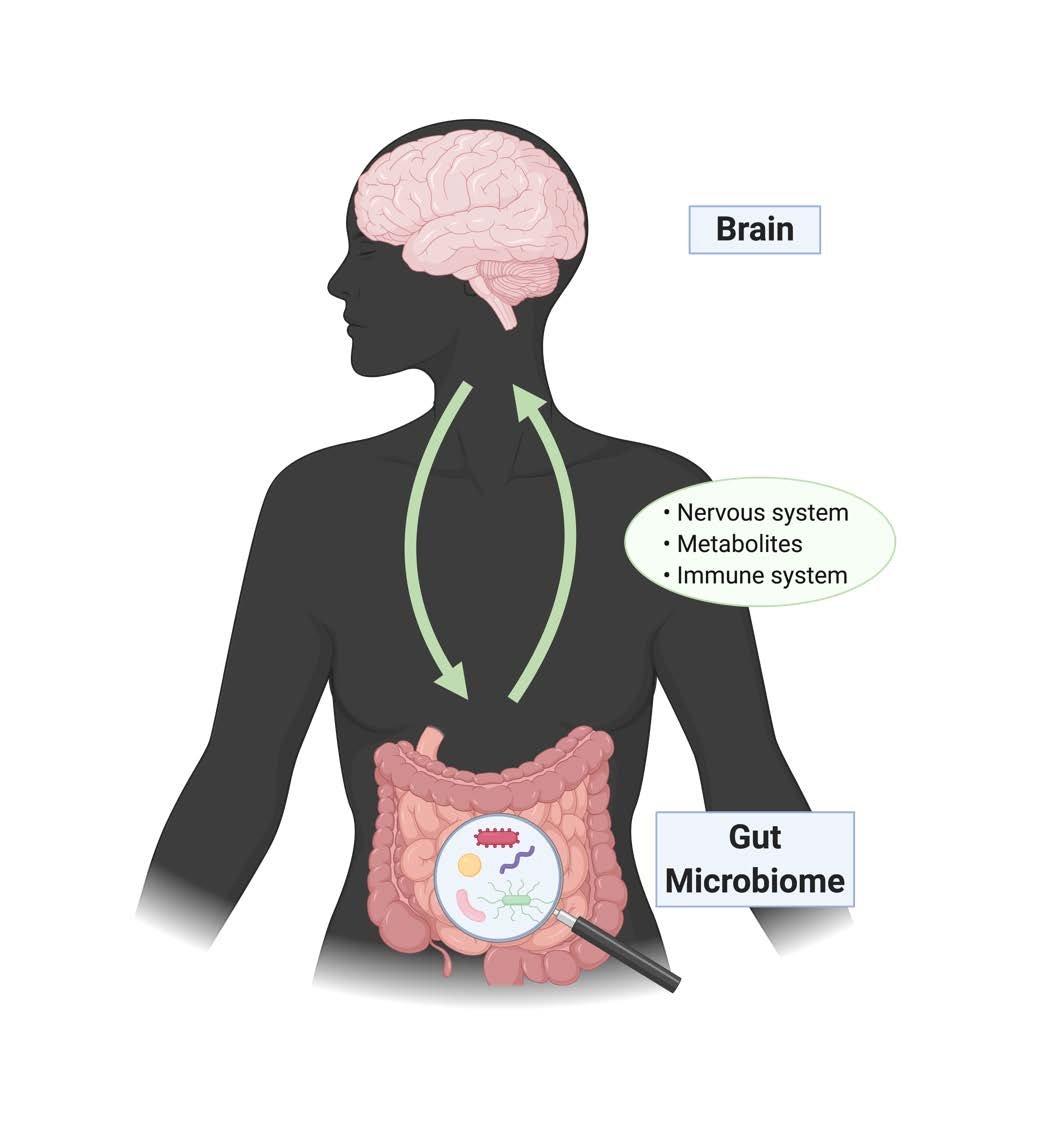
The gut microbiome has far-reaching effects on overall health, even beyond the gut. Recent research shows that these microorganisms are able to communicate with the brain to affect brain function and behavior. For this reason, neuroscience research has turned its focus to the Gut-Brain Axis. Recent research has identified the importance of the gut microbiome in normal brain functions [1,2], and alterations to the gut microbiome have been suggested to contribute to different psychiatric disorders, including depression [3], anxiety [4], autism spectrum disorders [5], and addiction [6]. For example, a recent study published in Nature Microbiology demonstrated that people with depression had deficits in two specific gut bacterial species [7].
Researchers have discovered that the gut microbiome communicates with the brain via three major mechanisms: (1) direct communication through nerves that project from the brain to the gut, (2) microbiome-released metabolites that enter the brain, and (3) immune system responses that are triggered by the gut microbiome [8].
Investigating how the gut and the brain communicate might allow researchers to identify new and effective ways to treat different psychiatric disorders, perhaps through use of probiotics [9], fecal transplants [10] or other treatments targeted to the gut microbiome. These microbe-based treatments, termed “psychobiotics” by neuropharmacologist John Cryan and psychiatrist Ted Dinan, are promising potential avenues of treatment for various psychiatric conditions.
Key Terms
Microbiome: A community of microorganisms and their combined genetic material inhabiting a particular environment (e.g. the bacteria, viruses, archaea, and fungi living inside the gastrointestinal tract are called the gut microbiome)
Probiotics: Live microorganisms that, when consumed, may be able to restore/improve/maintain a healthy gut flora through interactions with commensal gut microorganisms.
Gut-Brain Axis: A biochemical signaling network allowing the bidirectional communication between the central nervous system (AKA the brain) and the gastrointestinal tract (AKA the gut).
Psychobiotics: Refers to both Probiotics (defined above) and Prebiotics, which are compounds that enhance the growth of beneficial commensal gut bacteria. When ingested, these compounds are able to improved mental health outcomes through interactions with commensal gut bacteria11.
Citations
Cryan, J. F. & Dinan, T. G. Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience vol. 13 701–712 (2012).
Dinan, T. G. & Cryan, J. F. The Microbiome-Gut-Brain Axis in Health and Disease. Gastroenterology Clinics of North America vol. 46 77–89 (2017).
Capuco, A. et al. Current Perspectives on Gut Microbiome Dysbiosis and Depression. Advances in Therapy vol. 37 1328–1346 (2020).
Foster, J. A. & McVey Neufeld, K.-A. Gut–brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 36, 305–312 (2013).
Vuong, H. E. & Hsiao, E. Y. Emerging Roles for the Gut Microbiome in Autism Spectrum Disorder. Biological Psychiatry vol. 81 411–423 (2017).
Meckel, K. R. & Kiraly, D. D. A potential role for the gut microbiome in substance use disorders. Psychopharmacology vol. 236 1513–1530 (2019).
Valles-Colomer, M. et al. The neuroactive potential of the human gut microbiota in quality of life and depression. Nat. Microbiol. 4, 623–632 (2019).
Cryan, J. F. et al. The microbiota-gut-brain axis. Physiol. Rev. 99, 1877–2013 (2019).
Kim, N., Yun, M., Oh, Y. J. & Choi, H. J. Mind-altering with the gut: Modulation of the gut-brain axis with probiotics. Journal of Microbiology vol. 56 172–182 (2018).
Evrensel, A. & Ceylan, M. E. Fecal microbiota transplantation and its usage in neuropsychiatric disorders. Clinical Psychopharmacology and Neuroscience vol. 14 231–237 (2016).
Sarkar, A. et al. Psychobiotics and the Manipulation of Bacteria–Gut–Brain Signals. Trends in Neurosciences vol. 39 763–781 (2016).